Two drops of tears magnified the hardships in Taiwan's fight against the COVID-19 pandemic. Health Minister Chen Shih-Chung(陳時中) dropped his first tear when a case was confirmed on the charter flight that brought Taiwanese businesspeople home. The second was a tear of joy shed by the first coronavirus patient, a Taiwanese businesswoman, upon her recovery. These tears have united the Taiwanese people.
As the virus outbreak spun out of control in China and rapidly spread to Hong Kong and Macau, Taiwan was evaluated as an extremely high-risk area for COVID-19 due its frequent exchanges with the regions. Many Taiwanese also share family ties and relationships in China. As of May 25th, 91 cases of infection were confirmed in Taiwan. Fortunately, there has been no community transmission. Behind Taiwan’s success are thousands of invisible hands that have upheld the layers of virus prevention networks: they are the frontline hospitals and medical workers, the epidemic prevention team at the health ministry, the village offices, and the law enforcement.
The Reporter has visited the frontline to explore the foundation of Taiwan’s virus prevention and its hidden flaws behind the tears and challenges, as well as the risks and obstacles.
“I have to say this to all of the frontline workers: thank you for your hard work!”
After 16 days of treatment in isolation and three negative tests, a 55-year-old Taiwanese businesswoman recovered from the coronavirus and she was discharged from the hospital. She wrote the following letter to express her gratitude towards Taiwan’s epidemic prevention staff and medical workers:
“Imagine if you were well aware of the risk of infections and the dangers, would you do it? But the frontline nurses and the epidemic prevention staff had to come in direct contact with me for the fake of treating and helping me. When the weather was cold, they fetched me an extra blanket and hot water. If the food was cold, they heated it up in the microwave before sending it my way. When my lips cracked from dehydration, they contacted the doctors to get medicine and cotton swabs immediately. The doctors also explained my condition tirelessly and cheered me on. I am very, very, very thankful for you.”
She was the first coronavirus patient in Taiwan, also had the worst case of pneumonia. The director of the Hospital and Social Welfare Organizations Administration Commission, Wang Pi-Sheng(王必勝), was among the panel of physicians who treated the patient. He said the patient only had a mild fever, wet coughs, and shortness of breath, but her lung inflammation was worrisome.
The frontline medical team said they did not use Remdesivir, an antiviral drug that has gained newfound popularity, or other interferons for treatment. Aside from antibiotics, the team only used supportive treatments including cough relief, intravenous therapy, and oxygen delivery.
“But each day, we would contact the Central Epidemic Command Center (CECC) and epidemiology experts to confirm the patient’s conditions and medications. We are extremely cautious every step of the way,” they said.
"We have secured a case of recovery successfully," Wang said. He added that the Taiwanese patient had not only been discharged, she also never spread the virus to the local community. It was very encouraging for all the epidemic prevention workers. Behind this case of success, Taiwan had at least executed six layers of protection.
- Border control: to quarantine and test all passengers on the charter flight from Wuhan
- Airport epidemic prevention: temperature checkpoints at immigration and mandatory questionnaire
- Dedicated medical passage: the virus prevention team at the airport would contact the designated hospital should there be any suspected case of infection, and an ambulance would transport the patients directly to the hospital through a special passageway
- Public co-operation: passengers who notify the flight crew of their symptoms onboard and report at the immigration honestly
- Hospital infection prevention and control: establish a standard operating procedure for virus prevention and send patients to isolation rooms for treatment
- Expand investigation: track down passengers who came into contact with the patients, and monitor their home quarantine and self-health management procedures
Every process and system has been established gradually since the SARS outbreak left shocking lessons 17 years ago. Before SARS, some medical workers had never even seen an N95 mask. Since then, Taiwan has been holding annual drills and practices on epidemic command, hospital designation, infection prevention, and negative pressure isolation facilities. Taiwan is also among the few countries that has not canceled airport fever checks since the SARS outbreak, maintaining a level of alertness for immigration virus control.
Following SARS, Taiwan has seen six serious virus outbreaks including the H1N1 virus, the H7N9 novel influenza virus, dengue fever, and MERS. However, Taiwan has a relatively low number of virologists. The pending Public Health Professional Act has long been frozen at the legislature’s backend, further diminishing the number of public health specialists. In regards to its workforce development for epidemic prevention, Taiwan has only accomplished half of the setup.
Hundreds thousands are in home quarantine during the current COVID-19 pandemic. WHO experts estimated that the virus outbreak has not reached its peak. Taiwan is only relying on its limited epidemic prevention staff.

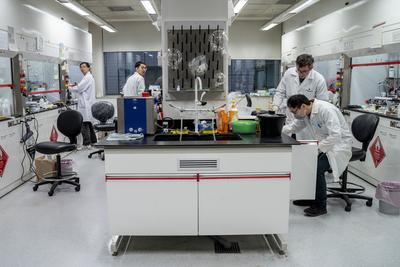
Taoyuan General Hospital, Ministry of Health and Welfare, is the closest hospital to the Taoyuan International Airport. It is a designated emergency response hospital for emerging infectious diseases, and it has received the most patients with suspected infections during this coronavirus pandemic. As the gatekeeper for Taiwan’s virus control, the Taoyuan General Hospital directly receives all the patients who arrive at the airport with a fever. It has tried its best to quash the individual cases on the periphery of the metropolitan community.
Including its Sinwu Branch facility, the Taoyuan General Hospital has 13 negative pressure isolation rooms in total. Since January, the hospital has received over 70 suspected cases of coronavirus infections, the largest number for any given hospital in Taiwan. Four physicians in the division of infectious disease and four infection control specialists were put on alert a week before the Lunar New Year holiday, and they have been rotating shifts non-stop ever since.
Cheng Chien-Yu(鄭健禹), 43, director of the infectious disease division at the Taoyuan General Hospital, did not make it to the SARS battle, but he is standing at the utmost frontline of this pandemic with extra caution. “Since we have drills every year, we are quite familiar with the practice,” he said.
These drills involve professional “fake patients” who act out the symptoms of infectious diseases, testing how the relevant staff would respond and handle the situations. This not only includes the emergency room staff and the resident medical personnel, but also the hospital security and janitors. Everyone would be subject to spot checks and regular practices of the standard operating procedure.
For instance, when the hospital receives a suspected case from the airport screening, the emergency room has to notify units like infection control and cleaning crew. When the patient arrives at the hospital in an ambulance, she or he has to go through an independent fever screening station. A doctor would perform a basic diagnosis to determine the severity of the patient’s symptoms, and send any high-risk patient to ICU and negative pressure isolation room. Each path and elevator on the designated route from the entrance to the interior of the hospital is designed to minimize contact with the public and medical workers. The negative pressure isolation room examination includes having nurses trained for wearing and taking off hazmat suits, security sealing off the blockade line, and the cleaning crew procedures.
Despite sufficient preparation, suspected cases were flooding in the hospital, drastically increasing the pressure for the frontline medical workers. Arranging the availability of the negative pressure isolation rooms is especially challenging. Every suspected case, from reporting to in-hospital stay to discharge requires at least three to five days. If the patients are not cleared of infection risks, they must be isolated in the negative pressure rooms. However, other patients with diseases like tuberculosis would need isolation rooms as well. Hospital overcrowding is the biggest worry for medical workers.
Taiwan has 1,028 negative pressure isolation beds in total. As of February 6, the alerted cases have reached 1,307. All suspected patients are required to remain in isolation until their infection risks are cleared. The capacity of the isolation rooms is facing mounting pressure.
After the Lunar New Year holiday, the suspected patients sent to the Taoyuan General Hospital doubled. The hospital had to empty 15 rooms immediately to prepare for overcapacity in the negative pressure isolation rooms.
Nonetheless, more COVID-19 symptoms have surfaced. Some patients have a mild fever or no fever at all, making it difficult to distinguish from the seasonal flu symptoms. As the gray area between the two diseases grows larger, the challenge for diagnosis is also higher. Because of the similar symptoms, frontline medical workers have a hard time erasing their worries. Cheng said that when the frontline staff show flu-like symptoms, the fears would spread.
“We have meetings every day to report each item of preparation to the entire hospital. We even review the tedious items daily and announce them in our LINE chat group. Even then our colleagues would still be worried, so we can only keep picking up the phone to explain,” Cheng said.
Since the Lunar New Year holiday, three workers at the Taoyuan General Hospital have already shown symptoms of a fever. The hospital was alerted and put the caretakers in isolation immediately. Fortunately, all three of them had the flu and tested negative for the coronavirus.

“Hello, Mr. XXX? How are you today? What’s your body temperature?”
At 9 a.m., the entire virus prevention team at Changhua’s Bureau of Health is already in the office. A team of 11 members, each with a phone in their hand, stares at the screen with a long list of names while making calls one after another.
According to the CECC instructions, people in mandatory home quarantine or isolation need to stay home for 14 days without going outside. Health department staff would call those in home isolation twice a day to confirm their health conditions, whereas those in home quarantine would receive one phone call per day from their county or village officers.
In Taiwan, over 500 are in home isolation and several thousand are in home quarantine. In Changhua alone, 32 people are in home isolation and quarantine. At least 50 to 60 people are mobilized from the department of health, law enforcement, to the village office to coordinate the virus control efforts.
“These two groups of quarantined people are asymptomatic and await further observations,” said Wang Hsiao-chi(王曉琪), chief of the Disease Control Division at Changhua’s Bureau of Health. Once the people in quarantine show any symptoms, the local virus prevention team would notify the Department of Health. Wang’s section would then contact the hospitals to transfer the suspected patients for treatment.
In a workday of over eight hours, the staff is not only responsible for the monitoring calls and case referrals. What The Reporter saw was the health bureau staff staring at data on the screen while cocking their head to hold onto their phone. There was almost no breathing space between each call. Every member has to deal with dozens of phone inquiries and complaints.
In the village office, officers have to finish “checking in” with the village residents who are in quarantine before 10 a.m. every day, and report to the district office.
“Do you have a fever today? Cough? What about muscle pain? Just hang in there for a little while. Don’t go running around!” A village official said.
In her village, a couple were in quarantine for 14 days. She lives near the couple, who are her acquaintances, and it was easier for her to look out for them. “On the second day of the routine calls, I had just started speaking and she interrupted me, saying that they were healthy, everything was fine except they had nothing to do,” she said.
Another village official said, “I have a Taiwanese businessman quarantined in my village until February 5. He asked me today (February 4) if he could go out tomorrow because he was too bored.”
They all agreed that the most taxing work in virus prevention has been comforting the irritated residents and convincing them to isolate for 14 days.
“There were people who came running to the health bureau questioning why they couldn’t buy any face mask and people who called three times a day to ask why they had to be quarantined… Communicating with the public is part of our job as the virus prevention staff, but we haven’t taken a break during this time at all. We can’t even count the number of phone calls we have to pick up each day. We would really need the public to cooperate and show more confidence and support for the staff,” Wang said.

Although the government has deployed a vast number of frontline workers to monitor people in quarantine through phone calls, some have gone missing occasionally. On January 28, the CECC announced the addition of “smart surveillance” for people in home isolation and quarantine. The CECC provided mobile phones for over 2,000 people quarantined in Taiwan, tracking their locations through GPS and reminding them to stay isolated.
However, the mobile phone manufacturers had to supply a large volume of supplies with the GPS system fully set up. There was a four-day gap between the central announcement and the local implementation. The Reporter visited various local departments of health and discovered that the mobile devices announced on February 28 were not delivered until the night of February 1.
Delivering the mobile phones to people in quarantine is not only a task for the health departments and village offices, but also the National Police Agency. Changhua County Police Department’s Administration Division Chief Chen Shih-Mien(陳世面) explained that the civil affairs units and the department of health would first provide a list of names for mandatory quarantines, the police department would then designate local police stations for assistance. The chief police officers and deputy officers would assist other units to visit the individual homes to set up the phone tracking system and LINE groups among others.
This has added extra strength in quarantine enforcement. Deputy Director-General of the Centers for Disease Control (CDC) Chuang Jen-Hsiang(莊人祥) said that aside from monitoring the quarantines with phone calls, the SIM card is linked to the nearest reporting station and it would trigger a system alert if someone leaves the area.
Chen said the police stations have a phone that is connected to the mobile surveillance system. “If people go outside or turn off their phone, the mobile phone in the police station would ring in the ‘Mission Impossible’ music. For safety, we would go check if the people are home,” he said.
At the same time, the village officials and the health department units would also receive a notification and contact the people on alerts. People who may have violated the quarantine would also receive a text message warning about their unusual location. If they did go out without permission, they would be subject to legal penalties under the Communicable Disease Control Act.
As the pandemic spreads from China to the rest of the world, however, the border control has expanded to all visitors. All Individuals with travel history are subject to mandatory home quarantine for 14 days. “The volume of home quarantine has grown too large and we cannot deliver the mobile devices to everyone. Our policies will be adjusted,” Chuang admitted.
Despite an upgrade in quarantine equipment and standard, contacts between virus prevention staff and people under quarantine are unavoidable. Concerns were mounting for the government units outside of the medical system, including police departments and village offices. A village official recalled the day of receiving a mobile tracking device, when he went off to visit a home with three to four people from the police agency and civil affairs unit all dressed in masks and gloves. They stood out in the crowd.
“We have to deliver the mobile phone to him directly, test the location tracking system, and ask him to sign the quarantine agreement and stay home for a while. Why would these tasks be assigned to a village off?” he questioned.
Chen said that the police officers were worried about visiting private homes, hence they always wore full gear with masks and gloves. As soon as they completed the visit, they always washed their hands and sanitized with alcohol. “But we are having a hard time because of insufficient mask supplies. The entire police department has 2,900 staff members but the central government only allocated 8,400 face masks to us. These will be gone very soon! All of us are scrambling to find face masks since this is an urgent problem,” Chen said.

Taiwan has adopted a multitude of measures, from taking strict precautions against imported transmission and enforcing quarantines of different levels, to making unprecedented decisions such as sending charter flights to bring overseas Taiwanese home and delaying school openings. The government’s performance in combating this pandemic has been remarkable, according to Fang Chi-Tai(方啟泰), a professor at the National Taiwan University’s (NTU) college of public health who has been involved in the 2003 SARS outbreak.
The most visible efforts to the public are the CECC’s press conferences, which took place every day of the week till June 7th. The CECC announces the latest COVID-19 updates through live streams, which has also led to the explosive popularity of Health Minister Chen Shih-Chung(陳時中). CDC Director Chou Jih-Haw( 周志浩 ) and Deputy Director Chuang Jen-Hsiang( 莊人祥 ) have also been rotating to speak at the conferences and on 24-hour standby. Netizens have even launched an online campaign titled “Minister Chen Shih-Chung, please take a break.”
The Ministry of Health and Welfare has mobilized a team of virus experts, including Vice President Chen Chien-jen(陳建仁), NTU Vice Principal Chang Shang-Chun( 張上淳 ), NTU infectious disease physicians Huang Li-Min( 黃立民 ) and Lee Bing-Ying( 李秉穎 ). These professionals have taken turns in filming videos for the health ministry, educating the public about hygiene with topics like handwashing and face masks.
Centralized information, press conference, media appearance, and filming were all experiences from SARS.
“The ‘hottest’ time of our life must have been during SARS,” said Huang Fu-Yuan( 黃富源 ), the then-CECC deputy commander and now an honorary consultant physician at the Mackay Memorial Hospital. During the SARS outbreak, the government took over three TV channel sessions between noon, evening, and midnight for five minutes each. All TV stations would screen the “Virus Prevention Frontline,” featuring Huang, Chen Chien-Jen(陳建仁),, and Lee Ming-Liang( 李明亮 ) among others. The government program had record ratings and its popularity was comparable to that of Chen Shih-Chung. That precious experience has allowed them to understand the importance of communicating directly with the public and promoting information, and it has proven equally useful for tackling COVID-19.
Huang said, “I think this is a very effective strategy. The delivery of virus prevention information and public communication are extremely important.” This tactic has also curbed the spread of fake news, increasing public trust in the government.
During the SARS outbreak 17 years ago, Taiwan’s government agencies, including the CECC, were operating separately. Lee Ming-Liang( 李明亮 ) , who was appointed CECC commander amid the crisis, has openly said, “In the early days of SARS, the opposition and disharmony between the central and local governments were all too palpable.”
At the time, the ruling Chen Shui-Bien(陳水扁) central administration and Taipei Mayor Ma Ying-Jeou(馬英九), who was responsible for the hardest hit area, were managing the outbreak without coordination. The Ministry of Health held an I-am-going-to-watch-you-die attitude while the Taipei Department of Health director insisted on otherwise: “Even if I am dead, I won’t ask for help.” In the end, the infighting has indirectly caused the closure of Heping Hospital due to the uncontrollable spread of the virus, further harming the public.
The year following SARS, the government made substantial revisions to the Communicable Disease Control Act, redefining the management authorities for the central and local agencies. Based on the severity of an outbreak, the central government may establish the CECC and execute necessary policies on behalf of local authorities. In the past 17 years, from H1N1 to novel influenza to COVID-19, the central authority has established the CECC without hesitation. The centralization of information and policymaking during virus outbreaks has avoided history repeating itself.
The society’s fears of emerging infectious diseases have always been larger than the diseases themselves. A lack of clarity or various disinformation are detrimental to virus control efforts. During SARS, some media outlets falsely reported over 80 cases of infection within the Mackay Memorial Hospital and employees throwing out “bottled letters” to seek help. There was also exaggerated news such as water pollution in the Wanhua District being the source of infection. Disinformation presented unnecessary challenges to the CECC as the authorities were juggling multiple tasks to contain the virus.
The Communicable Disease Control Act was revised again in 2019. Penalties for spreading rumors or incorrect information concerning the epidemic conditions were raised substantially from below NT$50,000 to NT$3 million. At the end of January 2020, Taiwan’s police agencies have investigated more than 30 cases of coronavirus disinformation and 16 people have been arrested and transferred to prosecutors.
Kuo Hsu-Sung(郭旭崧), the principal of National Yang-Ming University, was stationed in the Taipei Economic and Cultural Representative Office in the United States as a public health consultant when SARS broke out. He returned to Taiwan to join the fight against the epidemic and then became the head of CDC in 2004. The media communication has been more advanced this time around, Kuo suggested. “Back then we had a spokesperson and the CECC commander speak to the press after each ministry had its independent meeting. What’s different this time is that all the ministries involved would show their faces to the media, which is an important way to assure the public that the entire government is working to manage the crisis.”

The government’s steady epidemic prevention procedure, policymaking, public communication, and data transparency in its COVID-19 response and execution have gained tremendous public trust. Hidden flaws, however, have remained in Taiwan’s epidemic prevention system. The lack of virology professionals and funding forced the CDC to come up with emergency epidemic response. But to combat infectious diseases, especially for novel zoonotic viruses like SARS, MERS, and COVID-19, long-term “enemy observation” is all the more crucial. To find “the hidden terrorists” at any time, Taiwan needs field epidemiologists and public health specialists, who would conduct epidemic investigation and monitoring on humans as well as animals.
“Everyone says epidemic prevention is like fighting a war, but we didn’t give this system the appropriate configuration that can measure up to war efforts. Among the 7,000 staff members at the U.S. CDC, nearly half of them are either physicians or Ph.D.s. Taiwan’s CDC has almost 1,000 members, but it has only enlisted around 30 epidemiologists after SARS,” Kuo said.
Currently, only 24 epidemiologists remain. In Taiwan’s highest government body for epidemic prevention, the ratio of epidemiology professionals is significantly low.
The difference between epidemiologists and clinicians is that epidemiologists do not carry out individual diagnosis but they are rather “for the people.” Epidemic investigation is about clarifying the source of infection for a group of people. Through questionnaires and statistics, epidemiologists would compare the differences between an infected patient and a healthy person. Variables like clinical symptoms, incubation period, and test results for stool and vomit, would help determine the reason for infection and ways of prevention and improvement.
Epidemiologists are already hard to find in Taiwan, but veterinary epidemiologists are even rarer. According to the CDC’s 2019 Zoonoses Training Report, novel zoonotic virus is a significant international public health concern. Taiwan’s epidemic prevention system is, however, “lacking the professional talent and field researchers in the study of human and veterinary epidemiology.”
Based on the Global Health Security Agenda, the report evaluated the manpower necessary for Taiwan’s epidemic prevention: 118 field epidemiologists and 12 trained veterinarians. How many does Taiwan have? The CDC’s response was “unable to determine” because this particular labor force is “too mobile.”
The problem of manpower allocation is due to insufficient funding. Preparation for epidemic prevention starts far before an outbreak and some investments may be invisible during normal times. Armies are to be maintained in the course of years but to be deployed in moments of emergency. “Our epidemic prevention funding has been insufficient for years. If there have been no outbreaks for several years, the funding is cut,” Kuo said.
Kuo said epidemic prevention can be separated into three categories: The first is the United States, which can “save itself and save the others”; the second is Japan, which can protect itself; the third is Taiwan, which struggles to protect itself and requires external assistance in a dire situation.
“President Tsai Ing-wen(蔡英文) once said, ‘Health for all, Taiwan can help,’ with the hopes of Taiwan rising above a third-tier country and being able to provide epidemic prevention labor resources for the entire Asia. In reality, we don’t have enough,” Kuo said.
Epidemic prevention needs not only clinicians but also public health talent. Taiwan Public Health Association Director Chen Pao-Chung(陳保中) said public health specialists are like community epidemiologists as they identify the risks and solutions from community groups and fill in any gap in the virus prevention efforts. This field has a less visible presence and the professional suggestions may come in bits and pieces, but they are especially useful in the process of epidemic prevention.
Since 2000, Taiwan has been advocating the Public Health Professional Act in hopes of establishing a licensing system for public health specialists and allowing them to enter the community. The bill had failed to go beyond its first reading after SARS and it has found no success in the past 20 years. The bill has just been passed in mid May and becomes the first one in Asia. While the act has seen 20 years of delay, the United States and the United Kingdom have already established a licensing system for public health specialists in 2003.
Chen pointed out that public health specialists can quickly sort through and identify the focal points for surveillance when the community sees a surge in home quarantines and isolations. The virus screening station at the airport can also benefit from the presence of public health specialists in addition to having regular physicians and nurses; they can observe the traveler ratios from each country, evaluate their risks, and decide whether to adjust the monitoring standards, etc.
When patients visit the hospital, their travel history would show up when they insert their healthcare IDs. “But public health people would see things like the patient’s companion. And in the hospital, aside from the patients and medical workers, there are volunteers, the cleaning crew, shops, and parking garage… They can target the traffic flow in the entire hospital and design a set of relevant prevention measures,” Chen said.
It is also worth noting that public health specialists can better perform “public communication” in communities, encouraging the citizens to be more receptive towards centralized messages and to cooperate. “A central authority’s communication can yield very different results between advising the public to stay alarmed during an epidemic and causing widespread panic,” Chen said. Public health specialists can provide timely comfort and instill confidence in the community, for example, during their assistance in enforcing home quarantine.
Unfortunately, due to the absence of licensing, most of the public health talent who have the professional knowledge would not stay working in the public health system. In the past decade, public health students have declined from around 4,000 to less than half of that number. This type of work is mostly carried out by health department workers who have a nursing background or alternative civilian servicemen in the field.
Chen said, “It’s not that the current manpower is doing a bad job, but that public health specialists can provide more and deeper analyses to minimize overlooked weaknesses in epidemic prevention.”
As the Public Health Professional Act passed in Legislative Yuan on May 15, more and more public health specialists will be seen in various areas in the coming years.

Besides the government’s efforts in epidemic prevention and the gradual investment in public health talent, everyone is a part of the “epidemic prevention system.” In addition to developing good hygiene habits, citizens are socially responsible for reporting symptoms, travel history, contact history honestly, as well as cooperating with self-health management and quarantine policies. Protecting others, after all, is protecting oneself.
Kuo said that a common conception during SARS was that “the government would protect me.” With rising public awareness and the growing flow of information, average citizens are starting to understand their responsibility in joining the epidemic prevention efforts. “This time around, a lot of people have dialed 1922 to report their symptoms willingly, which was unseen during the SARS outbreak,” he said. This is a significant change for the better.
However, panic buying of face masks and hoarding supplies also went out of control. “I’ve been working at the CDC for so many years and my only feeling is that, whenever I think we can tackle [a crisis] perfectly, there is always another lesson to be learned,” Kuo said. “Our citizens have generally been good, but we will still need to improve from panic buying of face masks.”
In an attempt to calm the face mask panic, Kuo, as the principal of Yang-Ming University, made a school announcement on February 6 to warrant NT$1 million in reminding that healthy individuals do not need to wear face masks at all times before a community outbreak. “To encourage Yang-Ming University faculties and students to cooperate with government advice: until an official announcement of community transmission, if any faculty member or student following government policies contracted the coronavirus, I will provide a compensation of NT$1 million,” Kuo wrote. As a former epidemic prevention official, he took the lead to express trust and cooperate with the government’s judgment.
No matter how advanced the technology is for strict surveillance, the epidemic prevention system requires public cooperation to achieve perfection. If someone in quarantine sneaks out and leaves the location-tracking mobile device behind, the efforts would be wasted.
“I would like to ask our citizens to do one thing: behave. Epidemic prevention is not achievable through quarrels, but through following the advice outlined by the CDC. We can make up for the flaws in the system together. We have to be honest about feeling ill so we can save ourselves, our family, and those around us,” the first recovered coronavirus patient in Taiwan called on the public to band together in a voice recording.
The SARS outbreak from 17 years ago taught Taiwanese to embrace the habits of frequent handwashing and wearing face masks in everyday life. Today, after 17 years, the epidemic prevention efforts have escalated, but the system needs to be strengthened by the government and requires cooperation from society on all fronts. Only when every individual becomes a solid part of the epidemic prevention cycle can we minimize the level of harm and risks for the recurring fights against novel diseases in the future.
The read the Chinese version, please click:〈【抗疫前線】首位2019新冠狀病毒病人出院背後,支撐台灣防疫網的雙手與缺口〉.
深度求真 眾聲同行
獨立的精神,是自由思想的條件。獨立的媒體,才能守護公共領域,讓自由的討論和真相浮現。
在艱困的媒體環境,《報導者》堅持以非營利組織的模式投入公共領域的調查與深度報導。我們透過讀者的贊助支持來營運,不仰賴商業廣告置入,在獨立自主的前提下,穿梭在各項重要公共議題中。
今年是《報導者》成立十週年,請支持我們持續追蹤國內外新聞事件的真相,度過下一個十年的挑戰。